Medicaid Programs Straining To Meet Needs Of New Enrollees
Under the Affordable Care Act, millions of low-income adults last year became eligible for Medicaid and subsidized health insurance for the first time. Now states face a huge challenge: how to deal with an onslaught of able-bodied, 18- to 64-year olds who haven’t seen a doctor in years.
“It took a lot of time and effort to enroll everyone, particularly those who were new to the system,” said Matt Salo, director of the National Association of Medicaid Directors. “The next big step, and the biggest unknown, is finding out exactly how this newly insured population will use the health care system.”
Until now, the vast majority of Medicaid beneficiaries were pregnant women, young children, and disabled and elderly adults. Relatively few able-bodied adults without children qualified, so states did not set up their Medicaid programs to treat them.
The newly insured, most of them young adults, have different needs. Though not as sick as existing Medicaid beneficiaries, the newcomers are more likely than the general population to have undiagnosed and untreated chronic illnesses such as diabetes and heart disease.
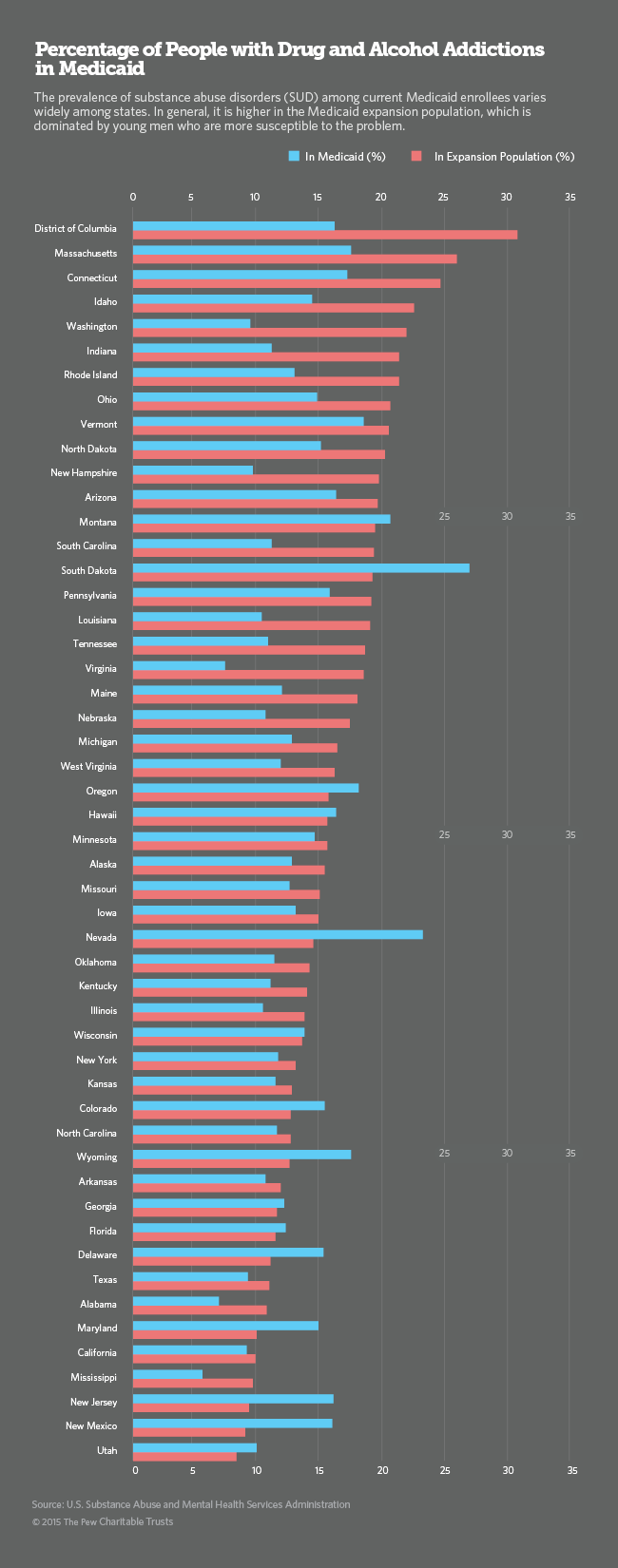
The starkest difference between the new population and the old one, however, is that the new enrollees have much higher rates of drug and alcohol addiction and mental illness.
Of the estimated 18 million adults potentially eligible for Medicaid in all 50 states, at least 2.5 million have substance use disorders. Of the 19 million uninsured adults with slightly higher incomes who are eligible for subsidized exchange insurance, an estimated 2.8 million struggle with substance abuse, according to the most recent national survey by the U.S. Substance Abuse and Mental Health Services Administration.
In addition to increasing the number of people with health insurance, the ACA for the first time made coverage of addiction services and other behavioral health disorders mandatory for all insurers, including Medicaid. As a result, the number of Medicaid enrollees receiving addiction services is expected to skyrocket over the next two years.
Although Medicaid and other state and federal programs historically have provided care for people with serious mental illness, coverage of addiction treatments has been spotty. Optional under Medicaid until now, coverage in most states was limited, typically just for pregnant women and adolescents.
“It’s the biggest change in a generation for addiction services,” said Robert Morrison, executive director of the National Association of State Alcohol and Drug Abuse Directors. “Comprehensive addiction programs didn’t exist in Medicaid until now.”
Big Demand, Short Supply
Behavioral health professionals typically earn far less than other health care providers, in part because few insurers have been willing to pay for their services. Many who enter the profession quickly abandon addiction treatment for more lucrative specialties. The result: a national shortage of addiction treatment providers.
Now, as billions of insurance dollars from Medicaid and all other insurers are becoming available, behavioral health experts say it will take time, training and new state licensing policies to expand the pool of providers to meet the new demand.
“Providers are now having to run to be ready to bill Medicaid and insurance companies, negotiate contracts with managed care companies and understand what this new market looks like,” said Becky Vaughn, vice president for addictions at the National Council for Behavioral Health. “Medicaid directors are also hustling to catch up,” she said.
For more than two decades, the U.S. Department of Health and Human Services has handed out grants to states to pay for addiction services. Walk-in clinics and residential facilities treated indigents and people in the criminal justice system, as well as uninsured people who paid out-of-pocket on a sliding income scale. Insurance was rarely billed. “Now, venture capitalists are starting to say there’s money to be made,” Vaughn said.
The first step for states is to create ACA compliant addiction benefit packages and fee structures to compensate the mostly small businesses that currently offer detox and rehabilitation services. Longer term, states are expected to loosen current behavioral health licensing requirements and offer professional and business training to promote an expansion of the workforce.
A Growing Population
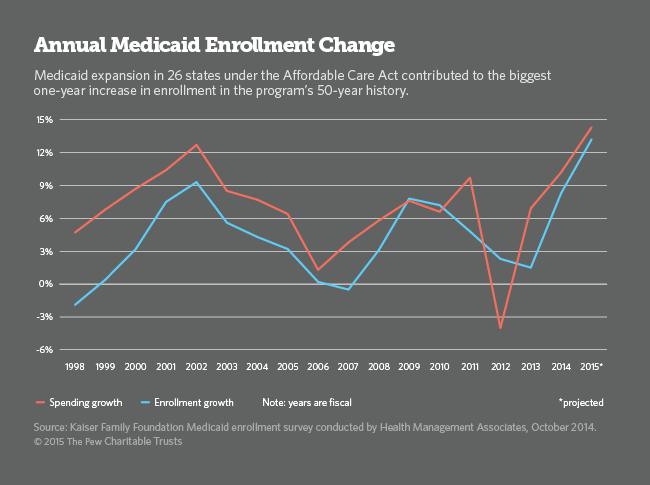
So far, 8 million people have signed up for exchange insurance policies and 7.2 million have enrolled in Medicaid since last year, according to the most recent data from the U.S. Department of Health and Human Services. Because Medicaid enrollment is continuous, those numbers are expected to rise substantially this year and next.
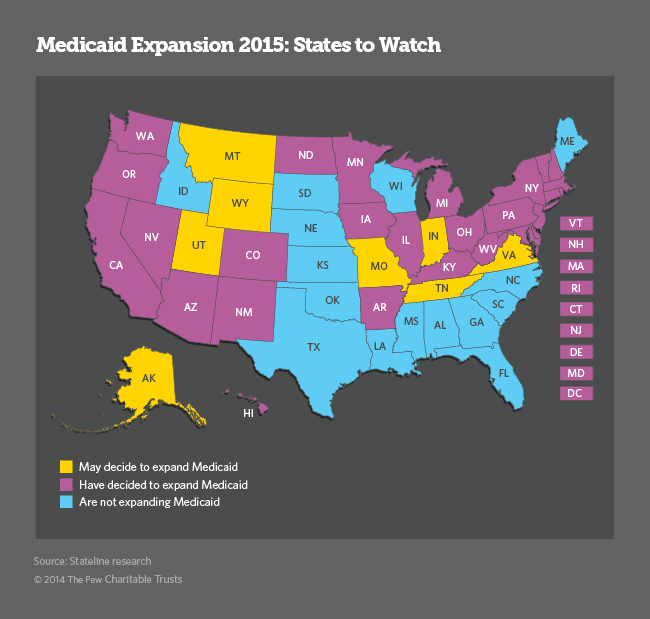
Under the ACA, states have the option of expanding Medicaid to adults with incomes up to 138 percent of the federal poverty level ($11,670 for an individual). The federal government will pay the entire bill for 2014 through 2016, and then it will pay a declining share over the following three years, and 90 percent thereafter. So far, only 27 states have taken up the option, but several GOP-led states are now considering it, potentially adding millions more adults to the Medicaid rolls this year.
Fourteen percent of the low-income adults who are newly eligible for Medicaid under the ACA have drug and alcohol addictions, compared to 10 percent in the general population. Because the new Medicaid population is dominated by young, single men—a group at much higher risk for drug and alcohol abuse—Medicaid enrollees needing treatment could more than double, from 1.5 million prior to the 2014 Medicaid expansion to about 4 million in the next five years.
Without treatment, their overall health care costs will be considerably higher. Compared to people without addictions, alcohol and drug abusers have poorer overall health. Their families often have poorer health as well.
Because of this, most Medicaid agencies want to find and treat newly eligible adults with substance use disorders as quickly as possible. The hope is that they will turn their lives around and move up the income scale and out of Medicaid altogether, said Salo of the Medicaid directors association. Medicaid officials also want to make sure people with addictions see a primary care doctor before their physical health worsens.
It’s not clear what portion of the adults who signed up for expanded Medicaid coverage last year have addiction disorders. In general, people with serious addiction disorders are not the first to sign up and maintain insurance coverage. Even less clear is when and whether they will seek help.
Low Treatment Rate
In 2012, about 22 million Americans were classified with a substance use disorder. Of those, 2.8 million had problems with both alcohol and drugs, 4.5 million had problems with drugs but not alcohol, and 14.9 million had problems with alcohol only. Only 2.5 million received help, according to the most recent National Survey on Drug Use and Health.
People with drug and alcohol problems are prone to deny that their substance use is a problem, and most tend to neglect their health even when they have insurance. The majority do not seek addiction treatment until they end up in crisis. When they or their families decide treatment is needed, it is often difficult to find a facility nearby that can take them.
“Up until now we have only had penetration rates of about 10% to 15% of the people who need services,” Vaughn said. “No other chronic disease would have that kind of low (treatment) rate.”
In the coming months, states and the federal government will begin releasing data, based on actual Medicaid claims, showing how many newly eligible Medicaid enrollees are using their new health cards, and for what. So far, there is only anecdotal evidence and limited state data.
In California, for example, 10,568 newly enrolled beneficiaries had signed up for addiction services by May, an increase of more than 30 percent under the state Medicaid program. The number of adults in Washington state’s Medicaid treatment facilities doubled in the first six months of the year. Vermont Medicaid officials also said they saw a substantial increase in the number of Medicaid enrollees seeking treatment.
Colorado’s director of health policy and planning, Susan Birch, said Medicaid officials there feared the worst but were “delighted” to find the 290,000 newly enrolled adults were healthier than expected. “We budgeted as if they would be in more of a dire, acute stage,” she said. “People aren’t coming in as sick as we thought and they’re not staying as long in our (Medicaid) system,” Birch said.
Part of the reason some Medicaid agencies are initially seeing milder cases of addiction is that many of the heaviest and most prolonged drug and alcohol users in Colorado and elsewhere have already ended up in jails, prisons and emergency rooms, or entered the state health care system as indigents.
In addition, many states have covered a limited number of addicted adults under special state-funded programs aimed at helping their poorest residents with severe mental illness and addictions. As a result, the number of new Medicaid enrollees with severe addiction cases, those that already have caused serious health problems, could be relatively low.
But states are no longer willing to wait for people to walk into a local clinic and ask for help. Instead, many state Medicaid agencies are working with primary care physicians and hospitals to reach people with addictions before their physical and mental health crumbles and their work and family relationships fall apart.
“We’re talking about those that are pre-catastrophic cases,” Birch said. “We hope we can keep people from getting worse before they get into the organ transplant and suicide realm,” she said. Colorado has launched a statewide collaboration program between primary care doctors and behavioral health specialists to ensure that happens.
A Huge Payoff
Much of the current emphasis on addiction services stems from medical research showing that individuals with untreated drug and alcohol disorders are among the heaviest users of the health care system, contributing to a substantial share of rising Medicaid, Medicare and private health care spending. Mounting evidence also shows physical healthcare costs decline dramatically when people with substance addictions get treatment. The longer they maintain sobriety, the lower their medical bills are.
“All of a sudden there’s a great deal of interest in people who are ‘high utilizers’ of emergency rooms and who don’t have any connection to healthcare,” said Art Schut, CEO of Arapahoe House, Colorado’s largest provider of drug and alcohol addiction services. “Many of the people we used to deal with didn’t have a primary care physician, and we couldn’t get them one,” he said.
A major goal for nearly all states is to find ways to better integrate physical and behavioral health, including addiction treatments. Now that addiction treatment is an integral part of Medicaid’s overall health plan, Schutt says he expects health outcomes to improve and costs to go down.
“We’re at the point where we’re actually treating substance use illness the way we treat other illnesses. There’s a realization in the commercial and public marketplace that health outcomes are important and that SUD (substance use disorder) treatment contributes significantly to overall health. It’s transformational for health care, not just substance use,” he said.
In Washington state, for example, the health agency invested in a drug and alcohol treatment program in 2005 and found that for every dollar spent, the state saved $2 in medical and nursing facility costs in the first four years.
“It’s hard for Medicaid directors watching mounting claims for addiction medications and treatments to take into account the expenses they’re not seeing,” said Morrison, director of the state alcohol and drug abuse group. But he said nearly every state agency is on board with the concept that addiction treatments, including medications, do result in substantial overall health care savings.
Colorado’s Schut says most providers already are trying to integrate physical and behavioral health, but until Medicaid agencies develop better financing options, their efforts will be hard to maintain. “The ACA opportunities are a dream come true,” he said, “but we’re not quite there yet.”
Stateline is a nonpartisan, nonprofit news service of the Pew Charitable Trusts that provides daily reporting and analysis on trends in state policy.






