Hospital Inspection Reports Released
A trove of recently released federal hospital inspection reports paints an uneven picture regarding the quality of care at California's hospitals.
The reports were compiled on hospitals at the behest of the Centers for Medicare and Medicaid Services during 2011 and 2012, and usually conducted by the California Department of Public Health. It is compiled in a new database, hospitalinspections.org, operated by the Association of Health Care Journalists.
According to the CMS, most of the inspections and reports were conducted and generated as the result of serious complaints.
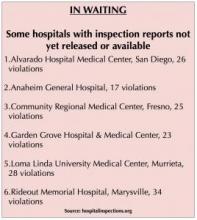
Four dozen reports were released on inspections that took place at California hospitals, detailing 199 separate violations of patient care or hospital operational protocols. Another 115 reports documenting more than 780 other violations have yet to be released, according to data posted on the hospital inspections website.
The available reports tell tales of improper monitoring of patients in intensive care units, expired drugs in use in hospital units, contaminated compounding pharmacies and patients restrained to their beds for days on end, among other incidents.
At least five of the reports detailed incidents that led directly or indirectly to patient deaths:
Â
- A November 2011 inspection at Alta Bates Summit Medical Center in Oakland discussed a 72-year-old patient with diabetes who died of a hypoglycemic incident because the nursing staff did not properly monitor her blood glucose levels.
- A patient being treated in the emergency room at UC San Diego Medical Center in February 2012 was found lifeless in a nearby locked restroom, having apparently swallowed an alcohol-based hand sanitizer. USCD Medical Center spokesperson Jackie Carr said that the gel-based hand sanitizers in use at the time of the death were switched to a non-alcoholic foam, and that dispensers could no longer be removed by patients.
- At Kern Medical Center in Bakersfield, a March 2011 inspection reported on a patient who died of head injuries sustained in a fall in the emergency room in September 2010. The patient had been in the ER for more than 40 hours prior to the fall. The hospital's medical director said the patient had “languished far too long in the (ER) without identified risks.â€
- A July 2011 inspection of Marin General Hospital in Greenbrae documented the death of a patient in May 2011 due to the use of a capped ventilator. Staff apparently ignored warning signs that the ventilator had not been properly connected. Proper followups by medical and nursing staff to avoid a repeat incident were not taken, according to the report.
- An April 2012 inspection of Tehachapi Hospital discovered that an 83-year-old ER patient died within minutes of her being discharged the prior month. The patient's vital signs were confused with those of another patient, and her records were not accurately recorded.
Two hospitals also received notifications of “immediate jeopardy†– that medical errors or conditions endangered the safety and lives of patients. The hospitals are required to submit swift corrective actions or risk being barred from the Medicare and Medicaid programs.
Stanford Hospital and Clinics received a notice of immediate jeopardy in March 2012 after a patient received three units of the wrong type of blood the prior month. The blood units had been intended for another patient. An investigation indicated the nursing staff had not followed proper procedures or engaged in correct documentation. Stanford officials agreed to clean up documentation and not keep patient labels in separate storage compartments.
At John F. Kennedy Medical Center in Indio, a May 2011 inspection led to the declaration of patients being placed in immediate jeopardy due to short staffing of its neonatal intensive care unit. At various times, only one registered nurse was caring for three “vulnerable†infants, including one suffering from sepsis and respiratory distress, according to the report. JFK officials agreed to beef up its NICU nursing staff as a result.
JFK Medical Center was also cited for failure to keep medications and foods at proper temperatures. In all, it received 25 violations during the inspection.
Fifteen separate violations were recorded during a February 2011 inspection at Los Angeles County-Harbor UCLA Medical Center, including the improper monitoring of the blood glucose levels of several adult and pediatric patients, the use of dust-covered humidifiers in operating rooms, and mislabeling of medications in storage areas.
A June 2012 report on Santa Clara Valley Medical Center in San Jose documented a vent in the operating room spraying non-sterile water onto the surgical wound of a patient undergoing a craniotomy.
A November 2011 inspection of Bakersfield Heart Hospital reported that a patient had been held in soft restraints for nine days in the prior month, despite physician orders saying the patient should not have been restrained longer than 24 hours.
Riverside County Regional Medical Center was tagged with a variety of violations that included unsafe medication monitoring procedures and keeping foodstuffs in the facility's kitchen long past their expiration date.
The database was released by the Missouri-based AHCJ during its annual meeting last week in Boston.Â
“Being able to easily review the performance of (a) local hospital is vital for healthcare journalists and for the public,†said AHCJ President Charles Ornstein, a senior reporter with the non-profit investigative journalism organization Pro Publica. Ornstein shared the 2005 Pulitzer Prize for public service journalism for his reporting in the Los Angeles Times on conditions at Los Angeles County Martin Luther King-Drew Medical Center.
In addition to obtaining the CMS inspection reports, the AHCJ has also tried to obtain certification reports from the Joint Commission. However, as a private agency, the Joint Commission has no legal obligation to release them under the U.S. Freedom of Information Act.
The AHCJ has implored the Joint Commission to release its inspection reports.
“The AHCJ board cannot accept the notion that patients are best protected by keeping hospital problems secret,†Ornstein wrote to Joint Commission President Mark Chassin, M.D. “Such reasoning also flies in the face of growing consensus among healthcare leaders and policy makers about the importance of transparency to improve medical care quality.â€






